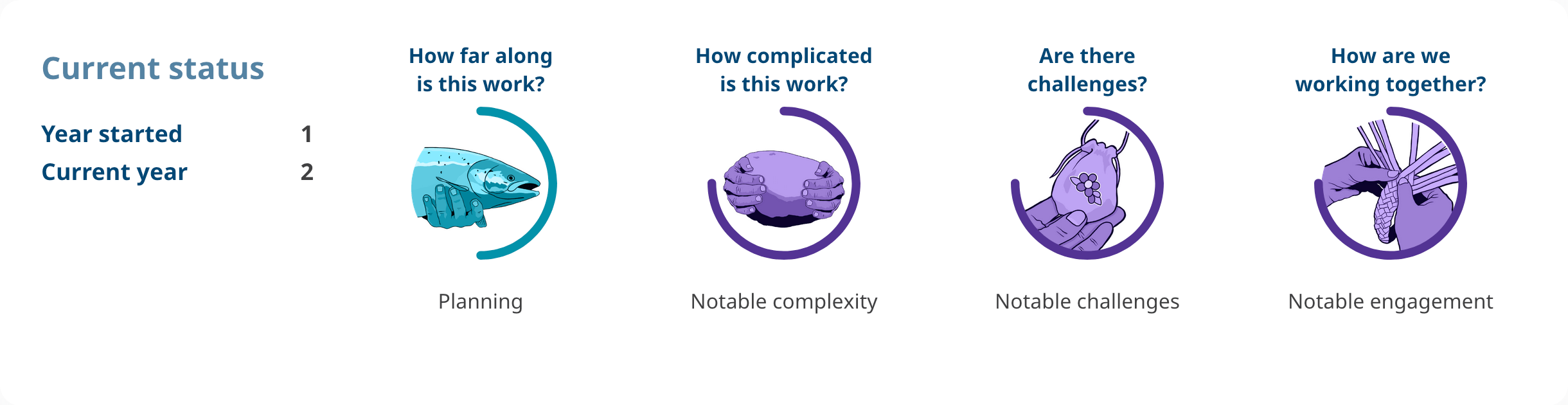
How are we working together?
The Primary Care Division in the Ministry of Health fosters strong collaborative partnerships with the First Nations Health Authority (FNHA) to enhance the delivery of primary health care services. Through regular engagement and joint planning, the Primary Care Division and FNHA ensure that virtual care programs are well supported, effectively implemented, and continuously improved. A key achievement has been strengthening the FNHA’s Medical Affairs and Wellness Office by enabling them to hold medical contracts for Indigenous-focused family physicians and nurse practitioners. This supports expansion of culturally grounded physician and nurse practitioner care through the initiatives like the First Nations-led Primary Health Care Initiative, First Nations Virtual Doctor of the Day, and some Primary Care Networks.
Are there challenges?
Funding for Real-Time Virtual Support services is currently approved until 2025/26.
The Ministry of Health’s Primary Care Division, in collaboration with Hospital and Provincial Health Services, Health Sector Workforce and Beneficiary Services Division, and Finance and corporate services, is conducting further policy work on coordinated virtual services and establishing a long-term governance structure for Real-Time Virtual Support services before seeking base funding for 2026/27 and onwards.
The FNHA is experiencing physician recruitment issues for their virtual care lines, which results in barriers to service provision and underutilized budget spends. Physicians working these call lines are at capacity. The Primary Care Division is working with partners to create a recruitment strategy to resolve this issue.
Highlights
From implementation (April 1, 2020, for First Nations Virtual Doctor of the Day and August 17, 2020, for First Nations Virtual Substance Use and Psychiatry Service) to March 7, 2025, there were 53,805 First Nations Virtual Doctor of the Day encounters and 8,385 First Nations Virtual Substance Use and Psychiatry Service encounters.
From April 1, 2024, to March 7, 2025, there were 11,057 First Nations Virtual Doctor of the Day encounters and 1,531 First Nations Virtual Substance Use and Psychiatry Service encounters.
Clients’ satisfaction rate for First Nations Virtual Doctor of the Day and First Nations Virtual Substance Use and Psychiatry Service:
- From patient satisfaction surveys from April 1, 2024, to March 7, 2025, over 90% of users accessing the First Nations Virtual Substance Use and Psychiatry Service report satisfaction with their appointment and over 92% of users indicate they would recommend the service to their family and friends.
- From patient satisfaction surveys from November 10, 2022, to March 7, 2025, over 95% of users accessing the First Nations Virtual Doctor of the Day service report satisfaction with their appointment and over 96% of users indicate they would recommend the service to their family and friends.
- From patient satisfaction surveys from April 1, 2024, to March 7, 2025, over 96% of users accessing the First Nations Virtual Doctor of the Day service report satisfaction with their appointment and over 96% of users indicate they would recommend the service to their family and friends.
- From patient satisfaction surveys from March 15, 2023, to March 7, 2025, over 91% of users accessing the First Nations Virtual Substance Use and Psychiatry Service report satisfaction with their appointment and over 93% of users indicate they would recommend the service to their family and friends.