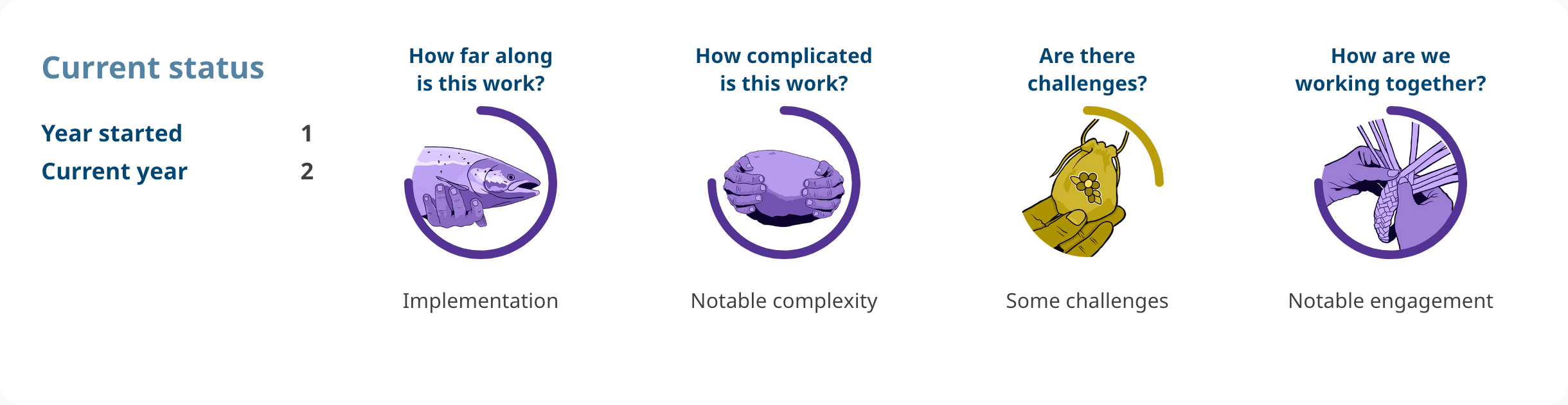
How are we working together?
The Ministry of Health continues to collaborate and engage with First Nations, Métis and urban Indigenous organizations throughout the various components of this action., including:
Decriminalization
- Law Enforcement Implementation Working Group, which includes the First Nations Justice Council and the Health Authority Working Group (First Nations Health Authority).
- Work with Métis Nation BC to be responsive to the decriminalization engagement needs of Métis peoples and communities.
- Building Relationships in Collaboration Grants committee (First Nations Health Authority, First Nations Justice Council and Métis Nation BC).
Harm Reduction
- Support the expansion of harm reduction initiatives through planning tables, oversight committees and working groups, including the overdose prevention services’ Minimum Service Standards development core advisory table. This work includes the First Nations Health Authority, Métis Nation BC, and the BC Association of Aboriginal Friendship Centres.
- As of July 2024, the Ministry of Health initiated service planning meetings with all health authorities and the First Nations Health Authority.
Youth Culturally Relevant and Safe Services
- Health authorities, the First Nations Health Authority, the BC Association of Aboriginal Friendship Centres, the First Nations Education Steering Committee and Métis Nation BC inform the implementation planning for integrated child and youth teams.
- The Province participates in regular Indigenous Partners Committee meetings with the First Nations Health Authority, Métis Nation BC, the BC Association of Aboriginal Friendship Centres and FNESC.
- The Province participates in monthly meetings with the First Nations Health Authority to support progress of Budget 2023 investments.
The First Nations Health Authority is also a key partner in harm reduction-related toxic drug crisis response and supports the regional response team. The health authority is involved in prescribed alternatives governance committees and working groups; is a key partner in the provincial drug checking network and in expanding access to opioid agonist treatment services; and sits on the implementation and steering committees that oversee certified practice designation for opioid use disorder.
Are there challenges?
Certified Practice designation for Opioid Use Disorder/Opioid Agonist Treatment
- First Nations have identified a need to provide programming that is community-led and Nation-driven, which builds on existing strengths and values of First Nations peoples and is not directed by other’s agenda or criteria. The First Nations Health Authority is exploring development of opioid agonist therapy programming that meets communities where they are at in relation to their specific needs, goals and beliefs around substance use.
Prescribed alternatives/harm reduction
- Partner capacity to engage with multiple streams of work at varying touchpoints may impact depth of engagement achieved. Mitigation of this risk is sought via close communication with key Indigenous partners.
Youth culturally relevant and safe services
- Integrated child and youth teams support new clinical and non-clinical roles hired in 20 school district communities across the province. Capacity to fully implement integrated child and youth teams and deliver services is dependent on available labour market resources and constraints.
Decriminalization
- There are unique challenges to expanding access to harm reduction initiatives, like drug checking, for rural and remote First Nations communities. The First Nations Health Authority will be working with regional health authorities and other partners to explore ways to mitigate these challenges.
- Disaggregated data is still needed to fully evaluate the equity impacts of decriminalization for Indigenous Peoples. The Ministry of Health continues to work with policing partners to improve access to this data.
- Since the new section 56 decriminalization exemption came into effect on May 7, 2024, possession offences have increased to approximately 2022 levels (pre-decriminalization). During B.C.’s original section 56 exemption, there was a 76% decrease in possession offences in the first year of decriminalization. More data is needed to understand this trend.
Highlights
In the month of December 2024, 44 overdose prevention services and supervised consumption services reported witnessed consumption visits to the BC Centre for Disease Control. Of these, 27 reported witnessed inhalation visits.
Starting in May 2024, the Province initiated a series of pilot projects exploring increased access to nasal naloxone to priority populations, including Indigenous People. Between January and June 2024, 2,415 nasal naloxone kits were distributed to 51 First Nations communities. In August 2024, 1,600 nasal naloxone kits were distributed to 25 post-secondary institutions and 25 First Nations Mandated Institutions. 50,000 nasal kits are being shipped to 150 community sites, as well as up to 700 pharmacies for distribution to people with dexterity limits, those in cold climates, youth, and Indigenous Peoples.
The First Nations Health Authority is supporting 68 First Nations communities, First Nations health service organizations and Aboriginal Friendship Centres to access public health vending machines and care cupboards to increase low barrier and 24/7 access to harm reduction supplies.
As of October 1, 2024, the certified practitioner in opioid use disorder scope of practice expanded to include an additional opioid agonist therapy medication, extended-release buprenorphine. With expansion, these practitioners can prescribe the four most common opioid agonist therapy medications in B.C. (buprenorphine, methadone, slow-release oral morphine and extended-release buprenorphine).