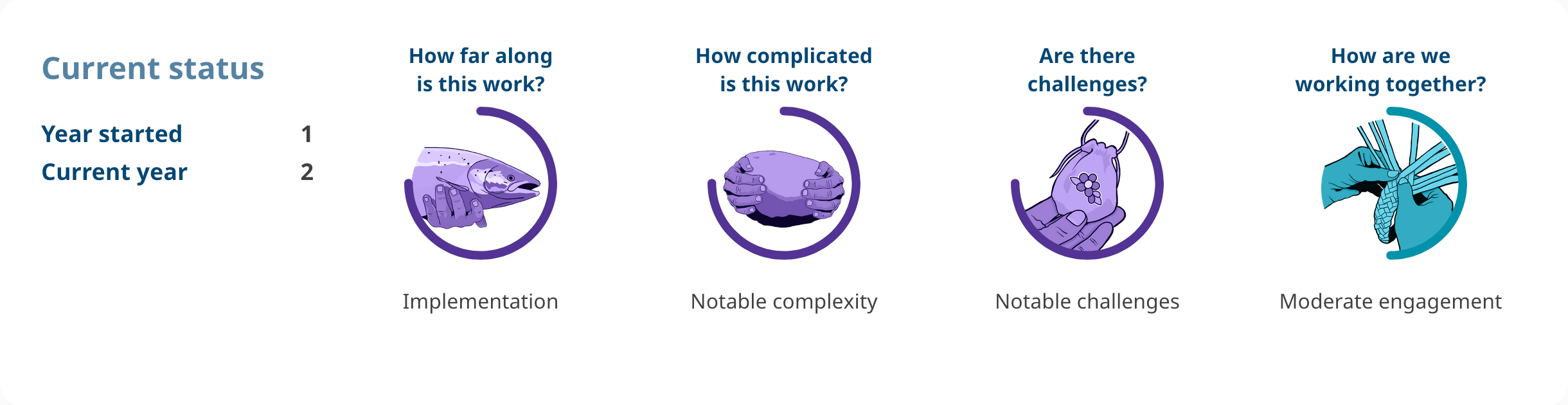
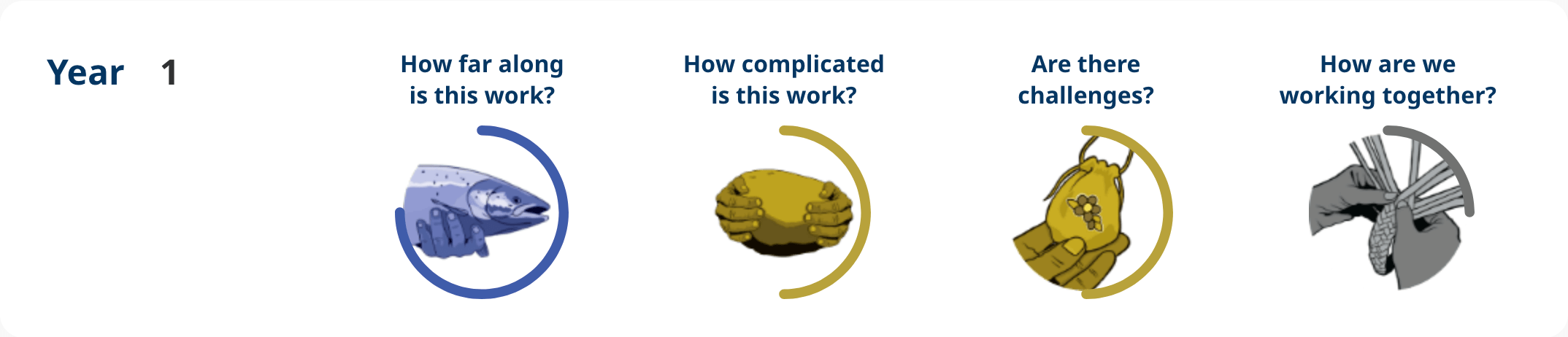
How are we working together?
The Ministry of Health is actively collaborating with the First Nations Health Authority (FNHA), who leads engagement efforts through close collaboration with local planning communities composed of First Nations health directors across the province. These committees are crucial in ensuring the planning and implementation of the Primary Care Networks and First Nations-led Primary Care Initiatives are culturally appropriate and aligned to the needs of Indigenous communities. Métis Nation BC and its Métis Chartered Communities are participating in some Primary Care Networks on Vancouver Island, with support of the Ministry of Health as part of the Indigenous Refresh strategy.
Are there challenges?
Primary Care Networks and First Nations-led Primary Care Centres have experienced service planning and implementation delays due to the health human resource shortages that significantly impacts progress in improving health care in regions throughout the province.
Additionally, increasing patient attachment gaps are commonly outpacing physician and nurse practitioner recruitment in Indigenous, rural and remote communities. Primary Care Networks and First Nations-led Primary Care Centres have experienced challenges with space planning as many sites require additional space and facilities to provide health care services to the communities in their respective regions.
There are also obstacles related to physician compensation and the requirement to provide full scope family practice in rural and remote communities. The Health Sector Workforce and Beneficiary Services Division and the Primary Care Division are working closely with the communities and regional health authorities to review practice category and direction moving forward to mitigate clinic closures.
Highlights
Qualitative feedback from First Nations, Métis and Inuit partners on Indigenous cultural safety and humility, learning, and engagement will be gathered through Primary Care Networks and First Nations-led Primary Care Centres. They will be incorporated into planning and implementation activities in ways that reflect the unique context of each local community.
Additional indicators regarding progress and outcomes as led and determined by Indigenous communities and organizations still need to be decided. The provision of physician services is created through locum work within First Nations communities. Furthermore, local community Primary Care Networks are engaging with First Nations and Indigenous health-serving organizations in service plan development and implementation. There are Indigenous representatives/representation within Primary Care Networks governance structures, including at planning and steering committee tables.
Representatives from each community are members of the Primary Care Network Planning and Steering Committees and are active in the Primary Care Network governance. In some cases, they serve as committee co-chairs. The planning and actioning recommendations of items result from engagement with Indigenous Peoples.
At the time of this report, there are 91 of 103 Primary Care Networks launched (88%) in B.C. There are 14 out of 15 First Nations-led Primary Care Centres approved, with three in operation providing services (All Nations Healing House, Lu’ma Medical Centre and Northern Nations Wellness Centre) and 11 in implementation (northern St’át’imc, Nlaka’pamux, Nuxalk & Ulkatcho, Fraser West, es zúmin’, Gitxsan & Wet’suwet’en Primary Care Centre, Dadzi Wellness Centre, Nuu-chah-nulth, Coast Salish, Éyameth’ Health Centre and Kwakwaka’wakw), and one in the service plan approval process (Fraser South).
Lu’ma Medical Centre, All Nations Healing House and Northern Nations Wellness Centre had 16,358 patient visits and 483 net-new attachments in the current fiscal year (between April 1, 2024, to December 31, 2024). Fourteen out of 15 approved First Nations-led Primary Care Centres aim to attach 26,950 new patients, with Fraser South planning to have an attachment target of an additional 3,200 patients.
According to the fiscal year 2024 and 2025 Primary Care Workforce Report current to January 2, 2025:
- 71.62/175.55 Full Time Equivalent (FTE) (41%) Indigenous Health resources (e.g., Elders and traditional wellness supports) recruited throughout all models of care (Primary Care Networks, First Nations-led Primary Care Centres, CHCs, NPPCCs, and UPCCs), supporting culturally safe team-based primary care delivery.
- 34.30/49.98 FTE (69%) recruited in three First Nations-led Primary Care Centres that are in operation.
- 60.20/245.04 FTE (25%) recruited overall in the 14 First Nations-led Primary Care Centres approved.